The notorious case of Campylobacter spp.: an overview of the increasingly antimicrobial-resistant foodborne pathogen
Author
Dipanjan Chakraborty
Hana Elbadawi
Amritanjali Kiran
Abhishek Kumar
Yara Mohsen
Lawrence Mugisha
Aparna Panicker
Maria Jose Ruiz Alvarez
Sajini Souda
Khine Swe Swe Han
Maarten Van Dongen PhD
Category
Pathogens, Microbiology
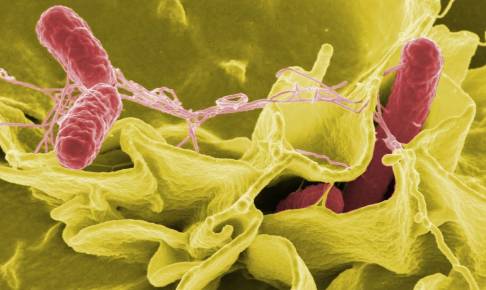
Why Campylobacter?
Campylobacter is one of the major foodborne pathogens of concern. C. jejuni and C. coli are the major causative agents, with C. jejuni accounting for approximately 90% of cases of Campylobacter-associated illness around the world (Tresse et al. 2017; Tam et al. 2003; Wieczorek et al. 2018). Campylobacteriosis caused by C. jejuni commonly causes severe diarrhoea, abdominal pain, fever, headache, nausea, and vomiting with some extreme cases resulting in Guillain–Barré syndrome (GBS) and acute flaccid paralysis (Havelaar et al. 2015; Ramos et al. 2021). Symptoms are severe in children below 5 years of age, the elderly, and immunocompromised individual. The infection is usually sporadic and self-limiting and thus does not require medication. Mortality due to Campylobacter infection is low (Mearelli et al. 2017). Campylobacter infection in humans is due to consumption of contaminated food and water (Tam et al. 2003).
Epidemiology of Campylobacter
Annually, approximately 800 000 cases occur in the Unites States of America alone, and the incidence in high-income countries varies from 4.4 to 9.3 per 1 000 people (Havelaar et al. 2015). In 2014, Europe reported a total of 240 379 confirmed cases from a total of 28 countries – an increase of 13% over the previous year (European Centre for Disease Control and Prevention 2017). In the Oceania region, Campylobacteriosis was the most reported foodborne infection in Australia in 2010, with 16 968 cases (Kaakoush et al. 2015).
Although surveillance data from developing countries is greatly lacking, Campylobacteriosis is endemic in certain parts of Africa, Asia, and the Middle East, especially in children under 2 years of age, who often have repeated or chronic infections (Kaakoush et al. 2015; Pascoe et al. 2020). Campylobacter infections rarely cause mortality, though occasional deaths occur in the elderly, immunocompromised, or paediatric populations (Kaakoush et al. 2015; Havelaar et al. 2015).
Geographical impact of Campylobacter
Campylobacter infection is zoonotic and it is present in domestic as well as wild birds and animals all around the world (Hald et al. 2016; Truccollo et al. 2021). Infection rates spike around summer in Nordic countries like Sweden and Norway (Kuhn et al. 2020). However, infection reports from Australia do not indicate an increase in the number of infections reported during the summer (Bi et al. 2008). The influence of weather and temperature on Campylobacteriosis is considered to be indirect as countries with high average temperature ranges like Nigeria (18 °C [65 °F] to 37 °C [98 °F] and countries with low average temperature ranges like Iceland (10 °C [50 °F] to 15°C [59 °F]) have reported cases of Campylobacteriosis, indicating that there is no correlation between temperature and the growth and spread of the Campylobacter species (Callicott et al. 2008). There are not many studies reporting the geographic, climate, and temperature impact on Campylobacter infections and the available studies do not show any significant correlation between geographical
Download content now